Retinal Detachment
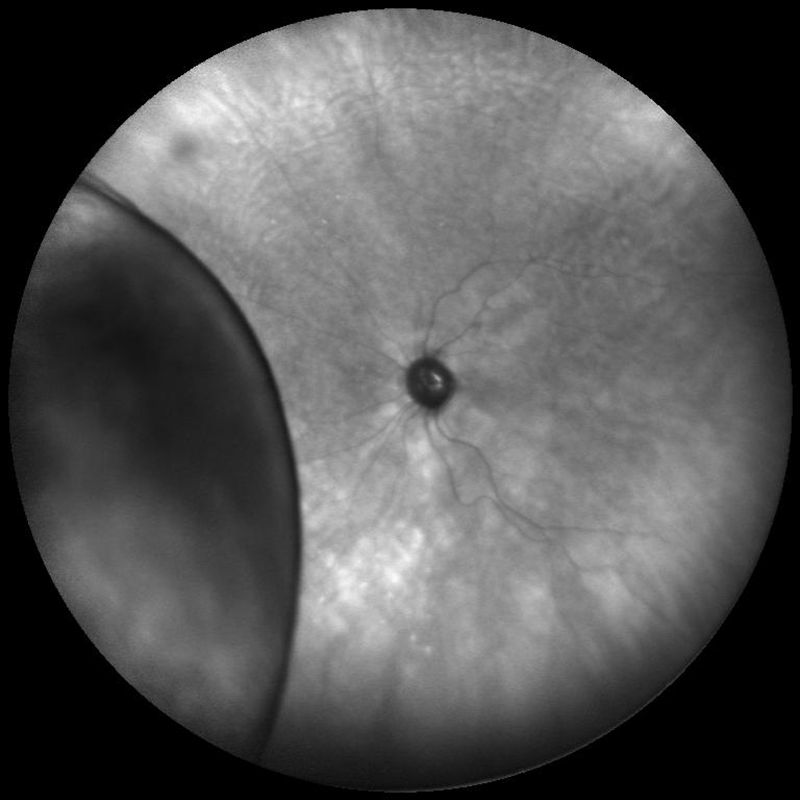 wide angle infrared fundus photo of a partial retinal detachment
wide angle infrared fundus photo of a partial retinal detachment
What is a Retinal Detachment?
The retina is the layer of specialized nerve tissue lining the back of the eye that allows you to see. The retina is very loosely attached to the back of the eye and in some cases, it may become detached. When the retina detaches, it is lifted from its normal position by fluid that accumulates between the retina and the eye wall. A detached retina is disconnected from its oxygen and nutrition supply, causing it to not work properly. After a retinal detachment, surgery is usually needed to return it to its normal position and prevent vision loss.
What causes a Retinal Detachment?
A hole or tear in the retina causes a retinal detachment. The presence of this hole or tear allows fluid to get underneath the retina and displace it from its nutrition source. Retinal detachments can develop at any age but tend to occur more commonly in the elderly. Retinal detachments usually occur around the time that the vitreous separates from the retina (PVD). Most PVDs cause no long-term damage to the eye, but in some individuals, they result in retinal tears that can then lead to a retinal detachment.
Who is at risk for a Retinal Detachment?
Anyone who has an increased chance of developing a retinal hole or tear is at risk for developing a retinal detachment. Detachments are most likely to occur in the elderly, but there are other factors that lead to an increased risk for a retinal detachment. These additional factors include people who are near-sighted (myopic), after an injury to the eye, after cataract surgery, or from weak areas in the retina. Lastly, detachments are more common in people who have a history of previous retinal tear or a family history of retinal tears or detachments.
What are the symptoms of a Retinal Detachment?
The symptoms of a retinal detachment are like those seen with a retinal tear or PVD. The first sign of a retinal detachment can be new floaters, intermittent flashing lights, cobwebs and perhaps a shower of black dots. Some people have prominent symptoms while others notice hardly anything at all. As the retinal detachment enlarges and detaches the retina near the center of the vision, a shadow or gray curtain can begin to move across the field of vision.
How is a Retinal Detachment treated?
Retinal detachments that result from a retinal tear almost always require surgery. There are several ways that a detached retina can be fixed. The type of surgery depends on the characteristics of the detachment. Some retinal detachments can be repaired in the office using a technique called pneumatic retinopexy and/or laser/cryotherapy, however most detachments need to be repaired in the operating room using a scleral buckle, a vitrectomy, or both. Laser therapy or cryotherapy (freezing) may be used to seal off a retinal tear or hole in patients with no detachment, or a very localized detachment. Pneumatic retinopexy also utilizes laser and/or freezing therapies in addition to the injection of a gas bubble into the eye. This procedure is used to reattach the retina and seal off the tear or hole. A scleral buckle surgery, performed in the operating room, involves placing a silicone band around the outside of the eye to provide permanent, external support to retinal tears or holes. Lastly, a vitrectomy surgery is a procedure performed in the operating room using tiny instruments inside the eye to remove the vitreous gel, reattach the retina and seal off all retinal tears and holes with laser or cryotherapy. Additionally, a gas bubble or silicone oil bubble will be placed in the eye to keep the retina flat until the eye heals. If gas is used, the eye will refill itself with clear fluid as the gas bubble reabsorbs over the course of a few weeks. If silicone oil is used, it may need to be removed surgically from the eye once the retina is stable.
Restrictions?
After surgery, most patients need to limit activity. It is common to have some mild discomfort after surgery. If a gas bubble has been placed in the eye, it is very important to maintain the proper head position. The success of the surgery depends on the position of the gas bubble. The eye naturally fills with fluid after surgery and will gradually replace the gas in the eye. While the gas bubble is in the eye, you cannot travel to higher elevations, fly in an airplane, or have specific types of anesthesia, such as nitrous oxide (“laughing gas;” commonly used by dentists). Any of these activities can lead to severe pain and possible blindness. Your retina specialist will tell you when it is safe to resume these activities.
Here is a great tool for patients who plan to travel or adjust elevations after having surgery:
Prognosis for my vision after treatment?
In general, with surgery over 98% of retinal detachments can be fixed. However, depending on the severity of the retinal detachment, some patients will need more than one operation to fully repair the retinal detachment. After the retinal detachment is fixed, vision can take months or years to improve. The overall amount of vision improvement after surgery is often impossible to predict. However, we know that vision improvement is less favorable in detachments affecting the central retina initially or those that have been present for a long time. Therefore, it is imperative to see your retinal specialist promptly if you note any flashes of light, floaters or loss of the peripheral (side) vision.