Age Related Macular Degeneration
 fluorescein angiogram of wet age related macular degeneration
fluorescein angiogram of wet age related macular degeneration
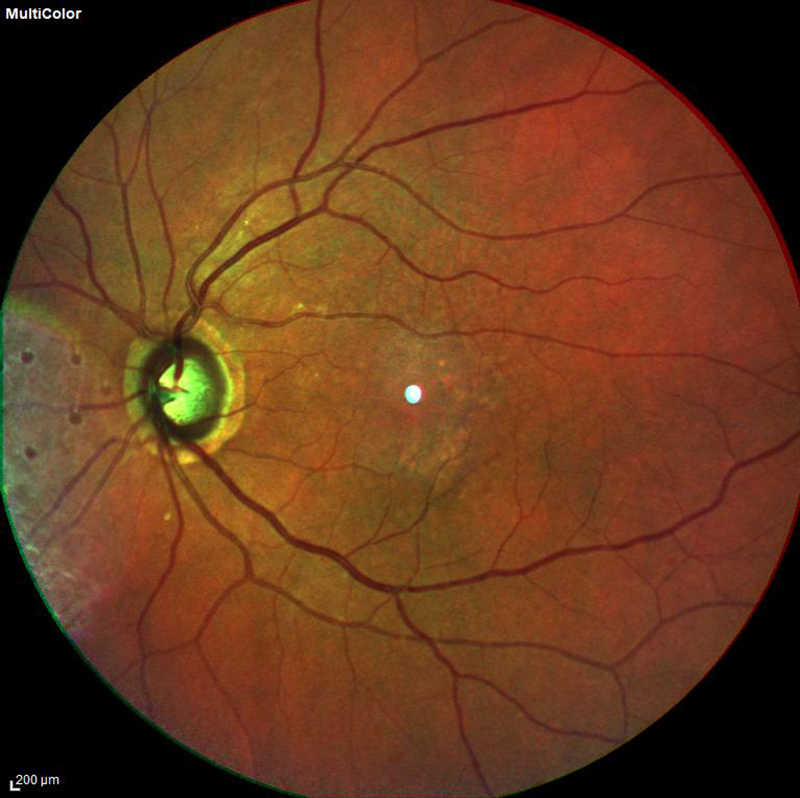 fundus photo of dry age related macular degeneration
fundus photo of dry age related macular degeneration
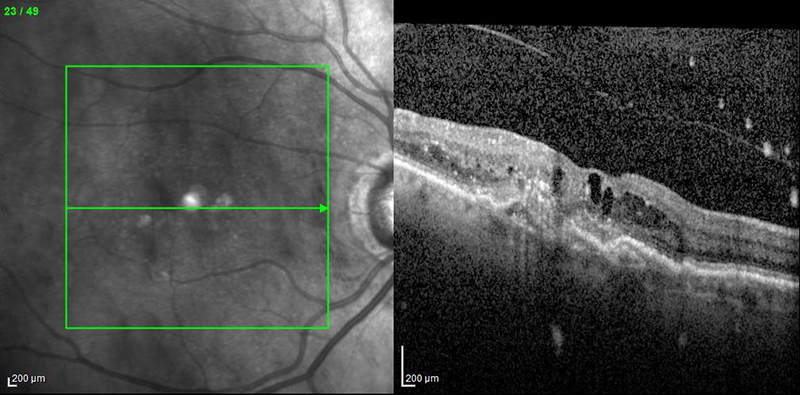 OCT of wet age related macular degeneration
OCT of wet age related macular degeneration
 fluorescein and indocyanine green angiogram of wet age related macular degeneration
fluorescein and indocyanine green angiogram of wet age related macular degeneration
 fluorescein and indocyanine green angiogram of dry age related macular degeneration
fluorescein and indocyanine green angiogram of dry age related macular degeneration
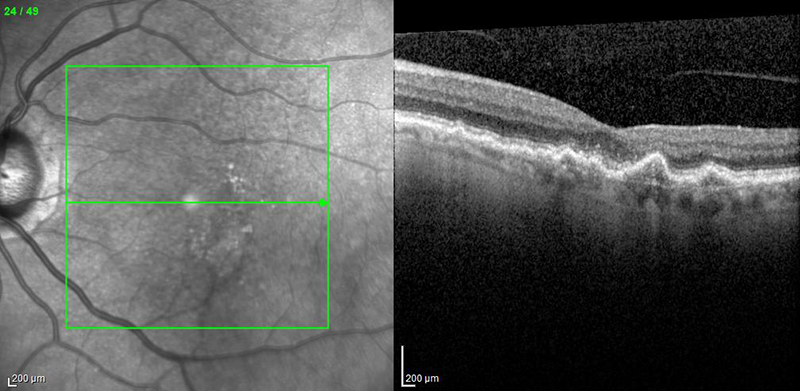 OCT of dry age related macular degeneration with drusen
OCT of dry age related macular degeneration with drusen
What is Age Related Macular Degeneration?
Age related macular degeneration (AMD) occurs when the macula is damaged. The macula is a structure that lies at the center of the retina, which is a layer of nerve tissue lining the back of the eye. The macula allows you to see fine details, both near and far. For instance, seeing the keys on a computer keyboard might be difficult for a patient with macular degeneration. Macular degeneration is one of the leading causes of vision loss in patients over the age of 50. It is typically non-painful and causes blurriness of your central vision but usually does not affect the eye’s peripheral/side vision.
Types of Macular Degeneration:
There are two types of macular degeneration: wet and dry. Patients with macular degeneration can have one, or both, of these conditions at the same time. The most common type, dry macular degeneration, is the cause of over 90% of cases of AMD. It is characterized by the formation of drusen, which is a yellow-colored material that forms underneath the retina. Sometimes, dry AMD can turn into wet AMD, where abnormal blood vessels grow into the retina. These blood vessels are very unstable and can break open, causing bleeding, swelling, and scar tissue. Wet AMD usually progresses quite rapidly, as compared to dry AMD, which is a slow-progressing condition.
What causes Macular Degeneration and am I at risk?
We do not know the exact cause of macular degeneration. We do know that as we age, the risk for having AMD increases. Some groups of people have a higher risk of developing AMD, including women, Caucasians, those that have a family history of AMD, and those with fair skin/blonde hair/blue eyes. Also, obesity, eating large of amounts of meat, cheese, and dairy, and smoking can all increase the likelihood of having AMD.
How do you diagnose Macular Degeneration?
Macular Degeneration can be diagnosed by your retina specialist, who will dilate your pupils with special eyedrops, so that he/she may examine the retina. Specialized testing, including an OCT (a special picture taken of the retina) and a fluorescein angiogram (a special dye injected to see the retina), can also be utilized in the diagnosis of macular degeneration.
What is the treatment for Macular Degeneration?
Depending on what type of macular degeneration you have, treatment differs. Unfortunately, there is no cure for macular degeneration, however please read below for the latest treatment options for this condition.
Dry AMD: While there are no specific treatments available, there are currently many clinical research trials being conducted to create new treatment options. Additionally, your retina specialist may recommend a special combination of vitamin supplements, AREDS 2 formula, as these are thought to slow the progression of advanced stages of AMD. The Age-Related Eye Disease Studies (AREDS & AREDS 2), which were large clinical trials, sponsored by the National Eye Institute (NEI), demonstrated a decreased risk of vision loss for people at risk of developing advanced AMD, by taking a combination of the following:
- Vitamin C
- Vitamin E
- Lutein
- Zeaxanthin
- Zinc
- Copper
Wet AMD: Since the early 2000s, there have been incredible advances in the treatment of wet AMD. Prior to that, a diagnosis of wet AMD carried a poor prognosis resulting in severe vision loss due to lack of suitable treatment. Fortunately, today there are several medications available that have been shown to benefit over 90% of patients with wet AMD. These medications primarily target VEGF (vascular endothelial growth factor), a molecule responsible for the growth of abnormal blood vessels which cause damage in wet AMD. Repeated injections of anti-VEGF agents (Avastin, Lucentis, and Eylea) have been firmly established as the optimal treatment for wet AMD. These powerful drugs are administered via injection into the eye and aim to suppress abnormal blood vessel growth and leakage. However, it is important to note that these injections are a treatment, not a cure, and often must be administered repeatedly (sometimes as often as monthly, indefinitely) to have their maximal vision-improving results. Other therapies for wet AMD include laser therapy and photodynamic therapy. Extensive numbing of the eye makes these treatment methods virtually painless.
What can I do to preserve my vision?
Patients with wet and dry AMD should check their vision regularly with a special tool called an Amsler grid. Please see the attached link below for a printable version of an Amsler grid. This tool can be printed on a special card or piece of paper and should be placed at eye-level, such as on a bathroom mirror or on a refrigerator. Next, stand about 1 foot away from the grid, cover one eye and look directly at the dot in the middle of the diagram with the uncovered eye. (Do not forget to wear your glasses!) Pay close attention, and note if any of the lines appear wavy, blurry or dim. Repeat the test with the opposite eye. Also do not ignore visual disturbances like new spots, blurring or smudgy areas within the central area of your vision, even if the Amsler grid shows no distortion. Call HRA if the abnormality is new or there is significant change in the vision.
Click here to download a printer friendly Amsler grid.
One should not only test his or her vision with an Amsler grid, but also remember to make healthy life choices, such as eating a diet with large portions of vegetables and fruits, with less saturated fat, avoiding smoking, and maintaining an active lifestyle and a normal body weight.