Idiopathic Parafoveal Telangiectasia (PFT)
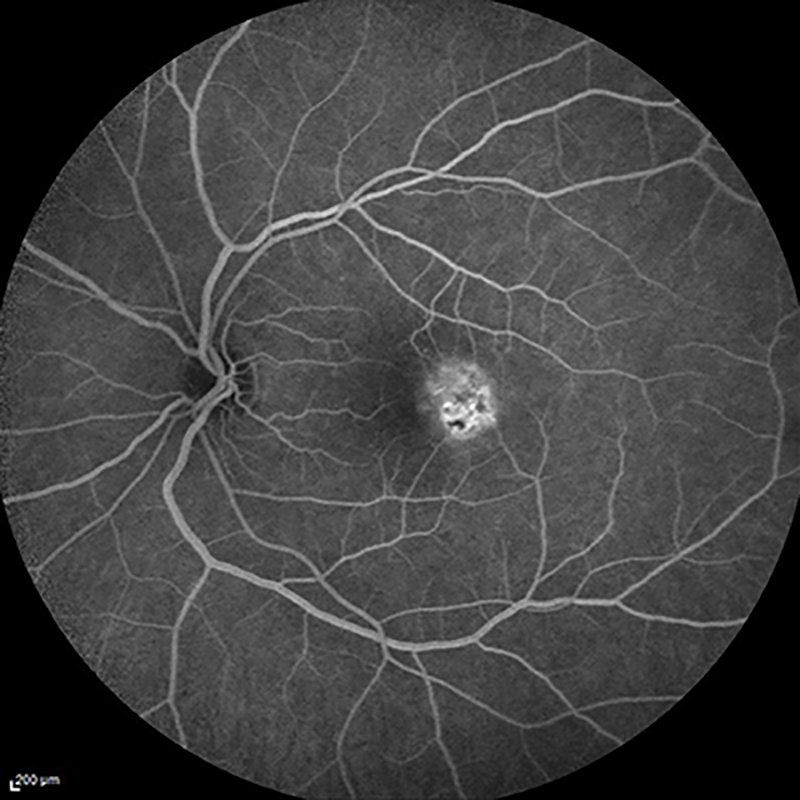 fluorescein angiogram of idiopathic parafoveal telangiectasia
fluorescein angiogram of idiopathic parafoveal telangiectasia
What is Idiopathic Parafoveal Telangiectasia (PFT)?
The fovea forms the center of the macula, the structure that lies along the back of the eye and is responsible for clear, detailed central vision. Parafoveal (“para-” = near), also known as perifoveal (“peri-” = around) telangiectasia or macular telangiectasia is an uncommon disease in which the capillaries and small blood vessels surrounding the fovea are abnormal and can cause vision loss. PFT can affect one or both eyes; however, it most commonly affects both. In some cases, the capillaries may leak, causing an accumulation of fluid called macular edema that can cause further decrease in vision. In other cases, abnormal blood vessels may grow, a process called choroidal neovascularization, which can leak fluid or blood into and under the retina, leading to scarring of the central retina and ultimately loss of vision if left untreated.
Am I at risk for developing PFT?
Parafoveal Telangiectasia usually occurs in individuals in their 50s and above. Often, these patients also have high blood pressure or diabetes. Lastly, some may have a history of undergoing radiation to the head and neck to treat cancer. Most commonly, the cause is unknown, or “idiopathic,” without a clear link to other conditions.
How is this condition diagnosed and treated?
A good way to detect PFT in its early stages is to look for the common symptoms. The most common symptom of PFT is gradual, progressive blurred central vision in one or both eyes. Other symptoms such as distorted vision or “blank spots” may occur. If you are having any of these symptoms, or notice a dramatic change in your vision, be sure to contact your eye doctor. Your eye doctor may then refer you to a retina specialist who will utilize a dilated eye exam, Ocular Coherence Tomography (OCT), and/or fluorescein angiography to visualize the affected structures of your eye. Treatment options include injection of specialized medications such as an anti-VEGF chemical (halts the growth of abnormal blood vessels) or other medications to improve your vision. Additionally, laser treatment is sometimes recommended depending on how your vision is affected. PFT rarely causes severe loss of vision and often can be managed with clinical observation.