Diabetic Retinopathy
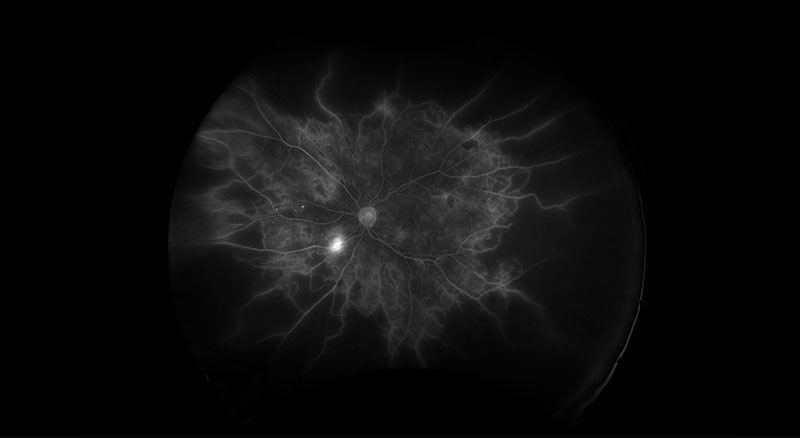 PDR Fluorescein Angiography
PDR Fluorescein Angiography
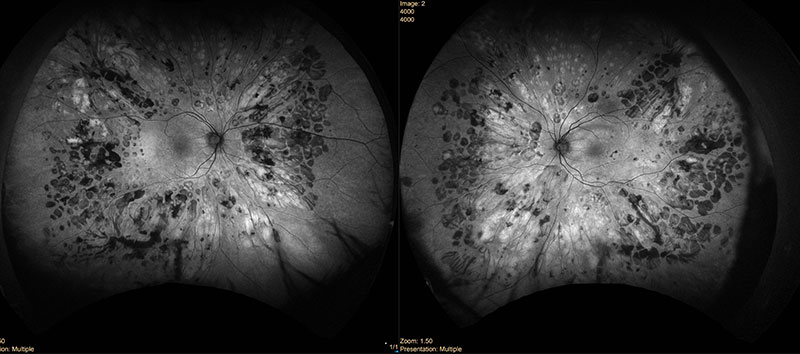 PDR Laser Autofluorescence Fundus
PDR Laser Autofluorescence Fundus
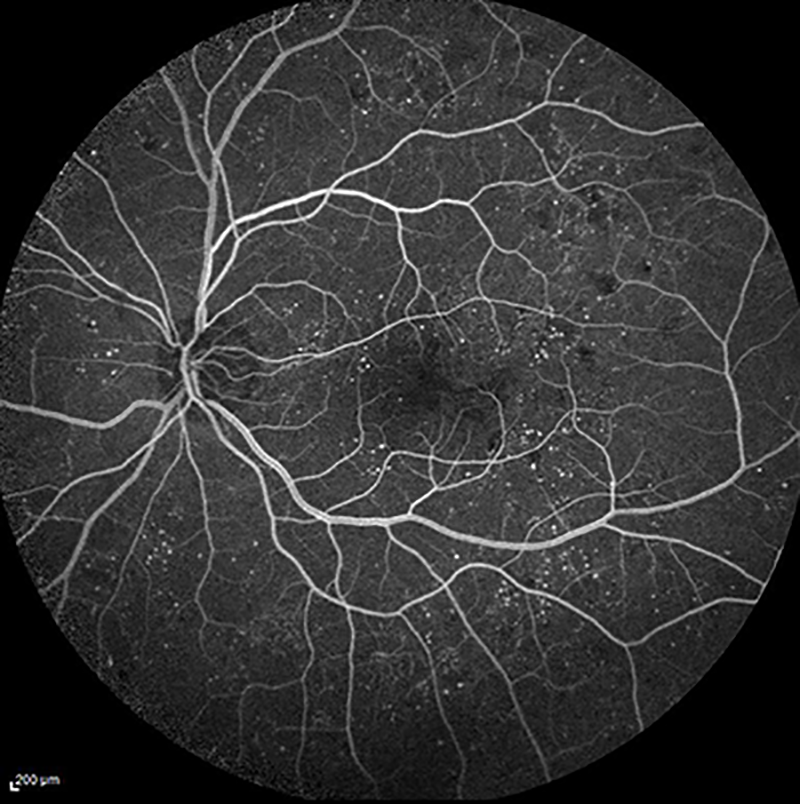 fluorescein angiogram of diabetic retinopathy with macular edema
fluorescein angiogram of diabetic retinopathy with macular edema
 fundus photo of diabetic macular retinopathy
fundus photo of diabetic macular retinopathy
 fundus photo of diabetic tractional retinal detachment
fundus photo of diabetic tractional retinal detachment
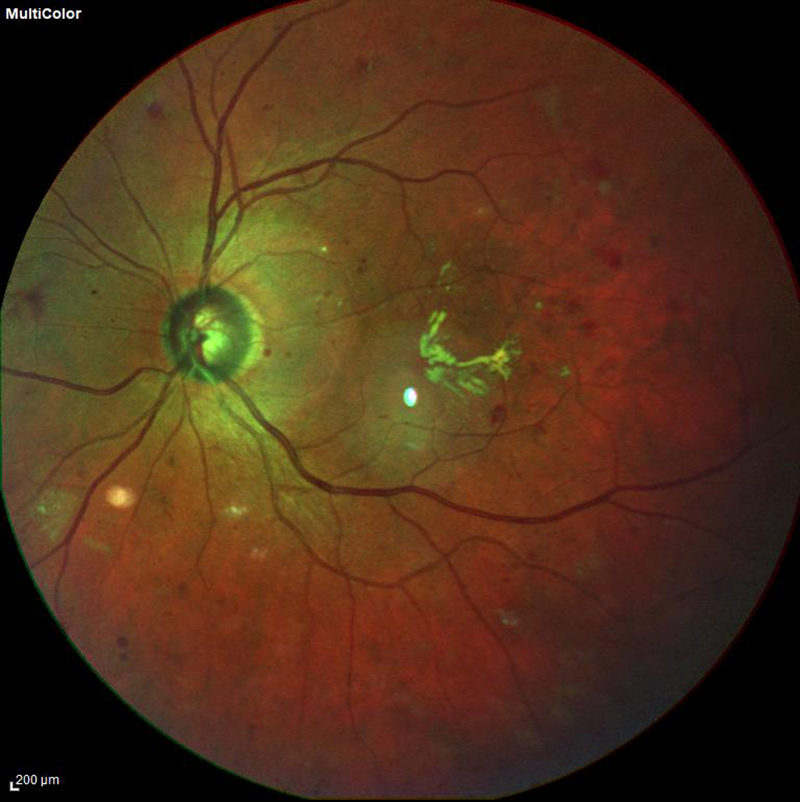
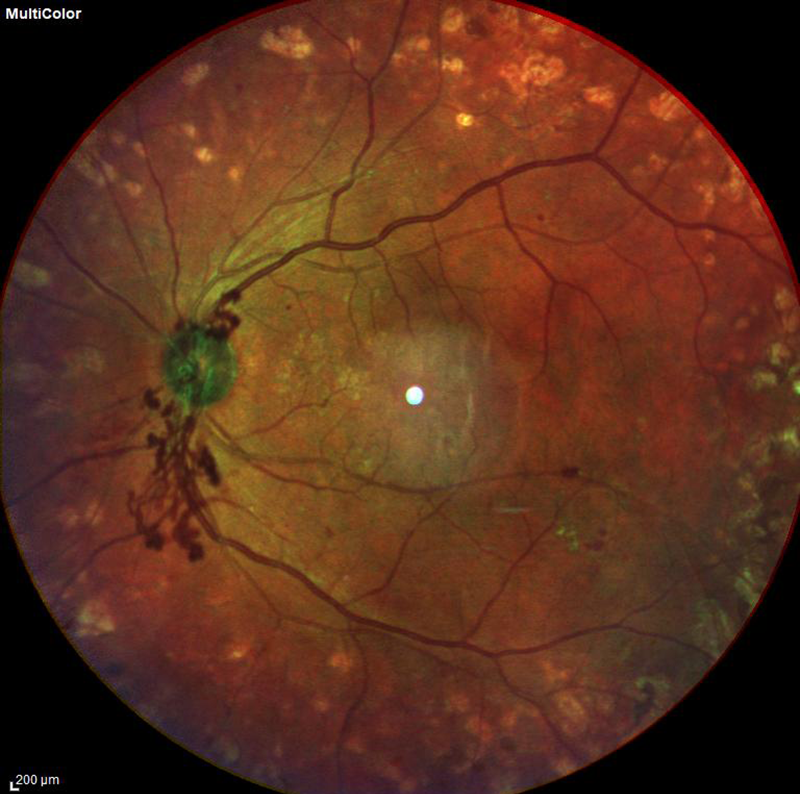 fundus photo of proliferative diabetic retinopathy with new blood vessels forming on the optic nerve
fundus photo of proliferative diabetic retinopathy with new blood vessels forming on the optic nerve
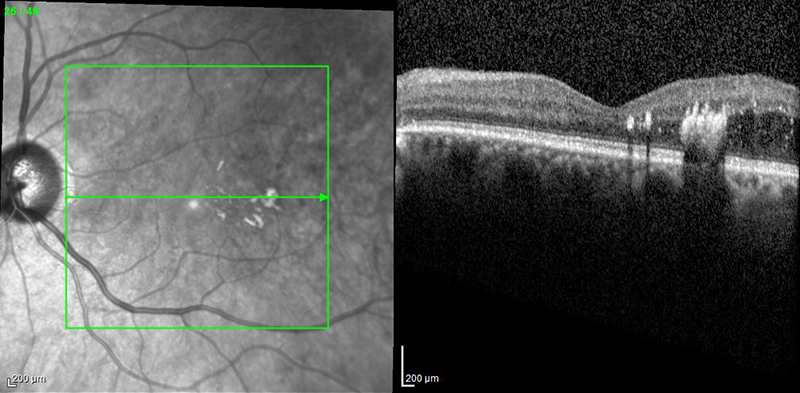 OCT of diabetic macular edema
OCT of diabetic macular edema
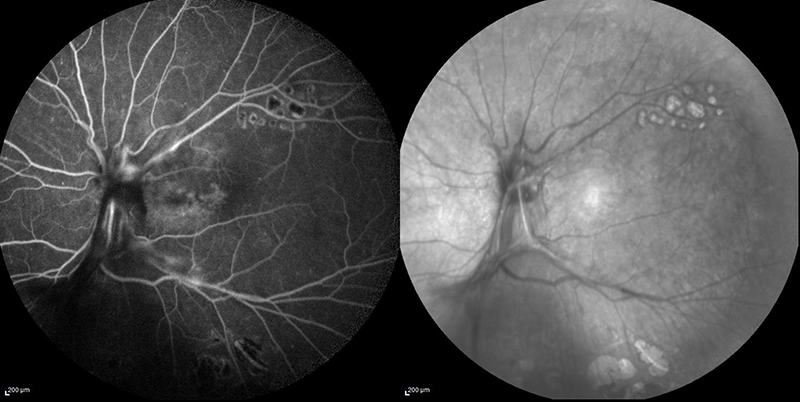 fluorescein angiogram and infrared fundus photo of diabetic tractional retinal detachment
fluorescein angiogram and infrared fundus photo of diabetic tractional retinal detachment
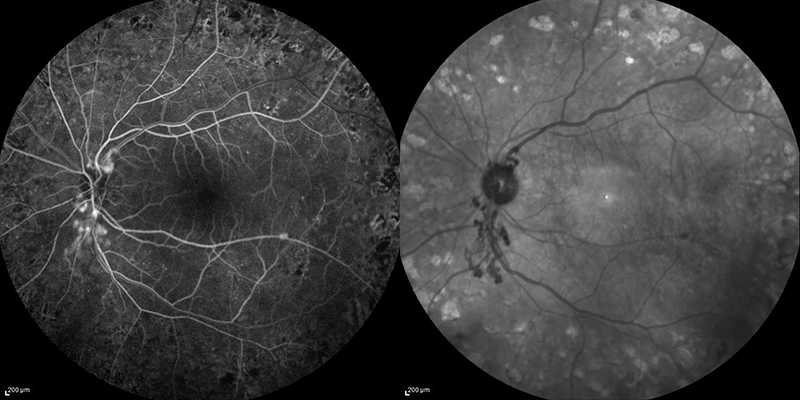 fluorescein angiogram and infrared fundus photo of proliferative diabetic retinopathy
fluorescein angiogram and infrared fundus photo of proliferative diabetic retinopathy
What is Diabetic Retinopathy?
Over half of patients with a history of diabetes can develop a condition known as diabetic retinopathy, which occurs when high levels of blood sugar cause damage to the blood vessels that feed the retina. We need healthy blood vessels to carry oxygen and vital nutrients to the retina, so that it can function to provide suitable eyesight. Diseased blood vessels may leak, become plugged, or begin to grow abnormally, all of which interfere with our eyesight. The longer you have diabetes, the higher the chance you will develop diabetic retinopathy. Severe vision loss or damage to the eye is more likely if your diabetes is poorly controlled. For unknown reasons, pregnancy can speed up the appearance of diabetic retinopathy.
What are the types of Diabetic Retinopathy?

ultrasound of a diabetic retinal detachment
There are two types of diabetic retinopathy: Non-Proliferative Diabetic Retinopathy (NPDR) and Proliferative Diabetic Retinopathy (PDR). In Non-Proliferative Diabetic Retinopathy, which occurs in the earlier stages of diabetic eye disease, the small blood vessels of the retina begin to leak and cause swelling. If this leaking and swelling occurs over the macula, it is called macular edema. If the swelling continues to progress, it can cause the blood vessels to close off completely, leading to macular ischemia, which will cause irreversible central visual loss that is not treatable and is permanent.
Proliferative Diabetic Retinopathy, a more advanced form of diabetic eye disease, involves the growth of new blood vessels in the eye. These additional blood vessels are problematic because they do not grow in an organized fashion and tend to bleed and scar, which can lead to floaters, poor vision, or a retinal detachment.
How is Diabetic Retinopathy Diagnosed?
You will have dilating eyedrops placed in your eye to widen your pupils, so that your retina specialist can examine the back of your eyes. You may undergo specialized testing, such as Optical Coherence Tomography (OCT), which obtains a high definition image of the retina. Another technique that is often used during exam is a fluorescein angiogram test, which is a dye test used to assess the blood vessels in the eye.
How is Diabetic Retinopathy Treated?
The best way to treat diabetic retinopathy is to carefully control your blood sugar. Checking your blood sugar regularly and maintaining tight control of your diet are very important here. You should also work closely with your primary care physician to control your blood pressure, weight, and cholesterol to achieve the best chances of maintaining your eyesight. Otherwise, early detection of the signs and symptoms of diabetic retinopathy is key to ensuring that early medical treatment is able to slow the progression of disease. For this reason, all diabetics should have at least one dilated eye exam per year.
Medical treatment options include injections of certain medicines into the eye. Medications called “anti-VEGF” drugs may be used, because they help to reverse some macular edema and new blood vessel growth described above. Sometimes, steroids may be used to treat any swelling associated with macular edema. Note, these medications generally need to be administered repeatedly for the rest of your life, as they usually provide only temporary relief of symptoms.
Additionally, laser treatment in the office may be used for patients with diabetic retinopathy to prevent further vision loss. The laser is used to help seal off blood vessels that are leaking and reduce swelling in the eye. Again, this will usually need to be repeated over time, as laser treatments are not meant to be curative. The main goal of all treatment modalities is to prevent further visual loss or worsening of your condition.
If you have excessive bleeding into the eye or a retinal detachment due to your condition, you may ultimately need to undergo vitrectomy surgery in the operating room. During this surgery, the vitreous gel (fills the inside of the eye), and any scar tissue in the back of the eye, is removed.