Macular Pucker/Epiretinal Membrane
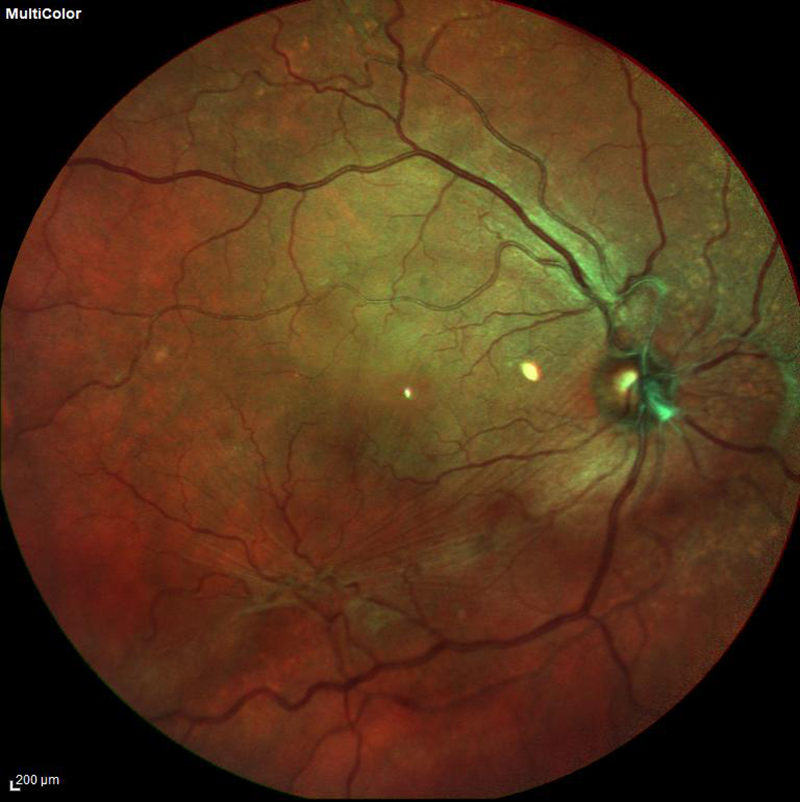 fundus photo of a macular pucker
fundus photo of a macular pucker
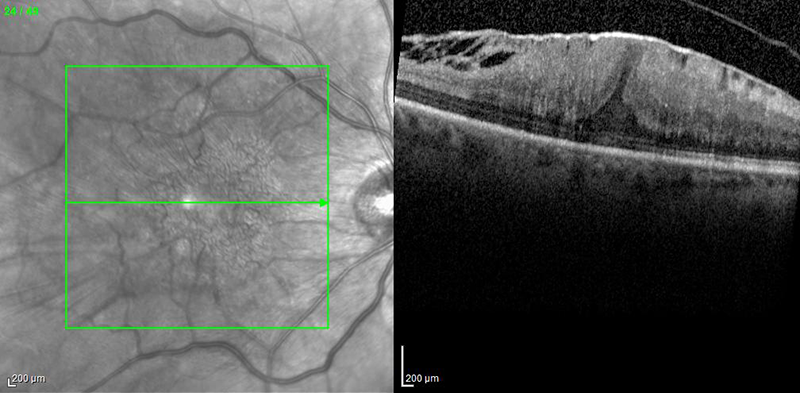 OCT of a macular pucker
OCT of a macular pucker
What is a Macular Pucker?
The macula is a specialized area of the retina and it is responsible for detailed vision. Usually the macula lies flat against the back of the eye. A macular pucker, also known as an epiretinal membrane, occurs when scar tissue forms over this part of the retina, causing the macula to contract and become ‘puckered,’ or wrinkled. This creasing causes swelling in the retina and visual disturbances.
What are the symptoms of a Macular Pucker?
A macular pucker can cause your central vision to be blurry, gray, or it can even cause a blank spot within your central vision. Straight lines, such as telephone poles, may appear wavy. Any task that requires detailed vision, such as reading or typing, can become difficult. The peripheral, or side, vision is not affected in this condition.
What are the causes of a Macular Pucker?
Usually, age is the most prominent factor leading to a macular pucker. As we age, the vitreous, or the jelly that fills the inside of the eye, can begin to shrink and pull away from the retina. Sometimes this tugging can cause scar tissue to form, leading to wrinkling or bulging within the macula and retina.
Other eye conditions can increase the risk of developing a macular pucker:
- Vitreous detachment (vitreous, or jelly, pulls away from the retina)
- Retinal detachment, or retinal tear
- Uveitis, or ocular swelling
- Diabetic retinopathy
- Trauma or damage to the eye (injury or surgery)
How is a Macular Pucker diagnosed?
Your retina specialist can diagnose this condition during a dilated eye exam. Further examination may be conducted with an optical coherence tomography (OCT – a detailed photograph of the eye) and a fluorescein angiography test (a test utilizing dye to look at structures within the eye).
How are Macular Puckers treated?
In cases that are accompanied by mild symptoms, often no treatment is needed. You may require different contact lens or glass prescription to improve your vision. If your symptoms are severe, you may need a special surgery called a vitrectomy with membrane peeling. This procedure involves using fine instruments to remove the scar tissue over the macula. This process helps to flatten the macula so that it returns to its appropriate position. For most patients, the vision will improve gradually after the surgery, however the vision may not be as good as it was prior to the macular pucker. The improvement will take several months. In some cases, the vision may not improve. It is rare for an epiretinal membrane, or a macular pucker, to reoccur once it has been surgically treated. Please remember that, as with any surgical procedure, there are risks involved with a vitrectomy, which you should discuss with your retinal surgeon.